Efficient Physical Therapy Charting: Tips and Best Practices
Physical therapy charting is crucial for quality patient care and compliance. This article explains what it involves, why it matters, and best practices for efficiency. Learn how proper charting can improve patient outcomes and streamline clinic operations.
Key Takeaways
Effective physical therapy documentation is crucial for patient care, legal compliance, and billing accuracy.
Key components of documentation include patient details, medical diagnosis, SMART treatment goals, and the SOAP note format.
Leveraging technology such as EMR software and voice-to-text tools enhances documentation efficiency and accuracy.
Efficient Physical Therapy Charting: Tips and Best Practices

Effective physical therapy documentation is the backbone of quality patient care and clinic success. Ensuring legal compliance, billing accuracy, and seamless communication among healthcare providers is essential. Without proper documentation, the risk of legal issues, billing discrepancies, and compromised patient care significantly increases. Avoiding these pitfalls requires documentation that is comprehensive, objective, and aligned with professional guidelines. This means eliminating irrelevant information, utilizing point-of-service documentation, and employing shortcuts like acronyms to streamline the process while maintaining essential details.
Quality documentation not only supports patient care but also ensures appropriate reimbursement for services provided. Summarizing the patient’s status and informing future treatment plans, documentation plays a pivotal role in a clinic’s success.
Utilizing the right software can further enhance the efficiency of charting, making sure that every note is thorough and accurate. We will explore the components of physical therapy documentation, common mistakes to avoid, and best practices for efficient charting.
Introduction
Charting in physical therapy is more than just a routine task; it’s a critical element that ensures the effectiveness of patient care. Proper charting captures every interaction and treatment outcome systematically, providing a clear and comprehensive view of the patient’s journey. This not only ensures that treatments are appropriate and aligned with the established plan of care but also safeguards therapists from potential legal issues and malpractice claims.
Using technology and best practices can significantly improve the efficiency and accuracy of physical therapy documentation.
Understanding Physical Therapy Charting
Physical therapy documentation is vital for legal compliance, billing accuracy, and ensuring continuity of care among healthcare providers. It encompasses the recording of a patient’s assessment, treatment, progress, and outcomes, ensuring effective communication and compliance. Quality documentation is not just about ticking boxes; it’s about providing clear, objective information that aligns with professional guidelines to facilitate better patient care and communication.
Physical therapy documentation should be comprehensive, objective, and adhere to professional standards. This includes using shortcuts like acronyms to streamline the process without losing essential details and employing point-of-service documentation to improve accuracy. Additionally, incorporating physical therapy documentation phrases can enhance clarity and consistency in records.
Eliminating irrelevant information enhances clarity and productivity, ensuring that every note is a valuable piece of the patient’s puzzle. Documentation should summarize the patient’s status, inform future treatment plans, and reflect treatment goals and specific interventions provided during each session.

Key Components of Physical Therapy Documentation
The foundation of effective physical therapy documentation lies in understanding its key components. These include patient details, medical diagnosis, treatment goals, and the plan of care. Each component plays a crucial role in ensuring quality patient care and legal compliance.
Documentation should include accurate patient information, a clear medical diagnosis, SMART treatment goals, and a detailed plan of care outlining future services and interventions.
Patient Details
Capturing essential patient details is the first step in effective documentation. This includes the patient’s name, date of birth, gender, address, and phone number. Additionally, documenting the patient’s medical history and medication lists provides a comprehensive view of their background, which is crucial for tailoring treatment plans. Key components also include the patient’s ID number, date of therapy, and session number.
These details provide context for the patient presents condition and inform treatment planning. For instance, knowing a patient’s past medical history, such as previous surgeries or chronic conditions, can significantly impact the approach to their physical therapy.
Accurate and thorough patient details ensure that all healthcare providers involved have the relevant information needed to deliver effective care.
Medical Diagnosis
Medical diagnoses are a crucial aspect of physical therapy documentation. It provides a comprehensive view of the patient’s background, helping healthcare providers understand the underlying issues that need to be addressed. Typically, a medical diagnosis is established by a physician prior to referring a patient to a Physical Therapist. A Physical Therapist cannot legally make a medical diagnosis, though they can provide a treatment diagnosis. Examples of medical diagnoses include specific codes like M17.12 for left knee osteoarthritis post total knee arthroplasty.
The distinction between a physical therapy diagnosis and a medical diagnosis is important. While the medical diagnosis identifies the condition, the physical therapy diagnosis focuses on the functional limitations caused by the condition. Understanding a patient’s previous physical therapy experiences can also inform future treatments and maintain an accurate treatment history.

Treatment Goals and Plan of Care
Effective treatment goals are essential for tracking patient progress and ensuring clarity in the treatment plan. The SMART format—Specific, Measurable, Achievable, Relevant, and Time-bound—is commonly used for this purpose. SMART goals facilitate the monitoring of patient progress and help in adjusting the treatment plan as needed.
The plan of care should include future services, specific interventions, patient education, and adjustments based on the patient’s progress. Outlining these elements ensures that every session aligns with the overall treatment goals, providing a structured pathway for recovery.
The SOAP Note Format
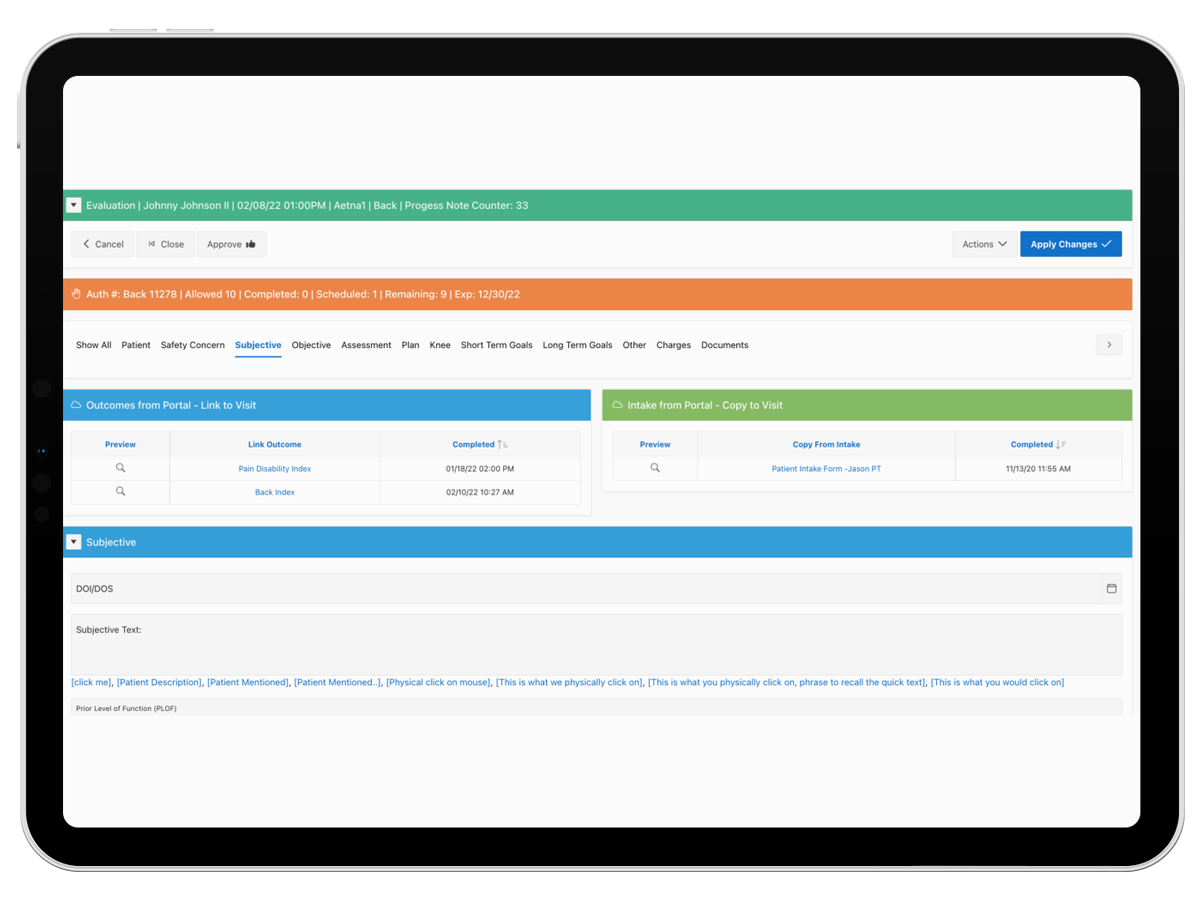
The SOAP note format is the most commonly used method for physical therapy documentation, helping ensure thorough and accurate documentation. SOAP is an acronym. It stands for Subjective, Objective, Assessment, and Plan. Each component plays a specific role in documenting patient care, from capturing the patient’s narrative to outlining the treatment strategy, including the physical therapy soap note.
Templates streamline the SOAP note process, making it more efficient and consistent.
Subjective
The subjective section of the SOAP note captures detailed patient narratives, including demographics, history, and personal experiences with their condition. This information provides context on the patient’s condition and informs treatment planning. Patients often report their pain levels, describe their experiences with their conditions, and note any recent changes in their health status.
Documenting patient self-reports is crucial for understanding their needs and tailoring care. For instance, a patient might describe their knee pain as a 7 out of 10, mentioning that it worsens after walking for more than 30 minutes. Such details are invaluable for devising a targeted treatment plan.
Objective
The objective section of the SOAP note documents observable and measurable data like test results or vital signs. This includes assessments of range of motion, strength, balance, and gait, which provide concrete evidence of the patient’s condition. For instance, recording that a patient has a hip extension of 20 degrees offers a clear, measurable insight into their physical capabilities.
Objective data is key for tracking patient progress over time. By comparing these measurements from one session to the next, physical therapists can determine the effectiveness of their interventions and make necessary adjustments to the treatment plan.
Assessment
The assessment section integrates data from both the subjective and objective parts to evaluate patient progress and the effectiveness of treatments. This is where physical therapists conduct a physical therapy assessment to interpret the collected data and form a clinical judgment. For example, noting that a patient has poor balance on an uneven surface might lead to targeted balance training exercises.
This section documents the therapist’s clinical reasoning and justifies the chosen treatment strategies. It provides a comprehensive overview of the patient’s current condition, progress, and areas that need further attention.
Plan
The plan section outlines specific treatment strategies, including interventions, frequency, and patient education, tailored to individual patient needs. This includes planned future services and any changes to the plan of care based on the patient’s progress.
By clearly documenting these elements, therapists ensure that each session is aligned with the overall treatment goals and that the patient receives consistent, targeted care.
Common Mistakes in Physical Therapy Charting
Common mistakes in physical therapy charting can significantly impact patient care and legal compliance. One frequent error is providing insufficient subjective information, which can lead to misdiagnosis and inappropriate treatment. Assumptions about a patient’s condition without thorough documentation can result in incorrect treatment plans.
Incomplete action plans in SOAP notes can hinder a patient’s progress and affect trust between the therapist and patient. Additionally, incomplete objective data can lead to misinterpretations, affecting treatment efficacy. Physical therapists must avoid using complex medical terminologies that can obscure essential information.
Over-documentation is another challenge, as it can dilute critical information and lead to inefficiencies. Ensuring clarity and precision in documentation is key to avoiding these common pitfalls.
Leveraging Technology in Physical Therapy Documentation
Embracing technology in physical therapy documentation can revolutionize how therapists capture and manage patient information. Physical Therapy Electronic Medical Records (EMRs) significantly enhance patient care and operational efficiency by streamlining documentation processes and reducing administrative burdens on therapists.
These systems improve accuracy and reduce documentation errors, which is vital for effective patient management. Leveraging technology ensures that documentation is thorough, organized, and compliant with professional standards.
EMR Software
Using specialized EMR software can optimize the documentation experience for physical therapists. For instance, ClinicSense is designed to enhance documentation quality and improve patient retention through features like appointment reminders. Cloud-based EMR systems offer flexibility and accessibility, making them a favored choice among physical therapy practices. Specialty-specific EMR systems provide tailored functions that align with the unique needs of physical therapy practices, ensuring that all aspects of patient care are accurately documented.
HENO EMR stands out by providing automated documentation for subjective, assessment, goals, and exercises, enabling quicker evaluations and compliance with Medicare requirements through integrated claims-based reporting. These features help physical therapists streamline their workflow, save time, and maintain high-quality documentation.
Voice-to-Text Tools
Voice-to-text technology is another valuable tool for therapists, allowing them to take notes quickly and accurately. By using voice-to-text tools, therapists can save time and reduce errors in physical therapy documentation, addressing the issue of over-documentation.
This technology ensures that every detail is captured efficiently, enabling therapists to focus more on patient care rather than paperwork.
Best Practices for Efficient Charting
Adopting best practices for efficient charting is crucial for maintaining accurate and timely documentation. These practices include timely documentation, the use of technology, and clear, objective language.
By implementing these strategies, physical therapists can enhance the quality of their documentation, ensuring it is comprehensive and compliant with professional standards.
Point-of-Service Documentation
Point-of-service documentation refers to documenting during or immediately after patient interactions, which can significantly increase the accuracy of charting. In home health settings, timely documentation after each session is essential for tracking patient progress and meeting insurance requirements. This practice helps maintain accuracy and detail in records, ensuring that all relevant information is captured.
By documenting at the point of service, therapists can ensure that their notes are fresh and accurate, reducing the likelihood of errors or omissions. This approach also allows for real-time updates to patient records, facilitating better communication among healthcare providers and improving overall patient care.

Use of Templates and Shortcuts
Utilizing pre-prepared templates and shortcuts can streamline the documentation process and save time. TextExpander, for instance, stores and quickly expands snippets, improving charting efficiency. When using shorthand in documentation, it is important to include a key for abbreviations to maintain clarity.
HENO EMR offers automated generation of subjective assessments, goals, and exercises, enhancing documentation efficiency and ensuring high-quality records. By leveraging these tools and techniques, therapists can focus more on patient care and less on administrative tasks, ultimately improving the overall quality of documentation.
Justifying Treatments Rendered
Providing thorough justification in documentation helps clarify the necessity of treatments and protects healthcare providers. This is essential to ensure that treatments are seen as necessary, effective, and appropriate, especially during audits or legal scrutiny. The following are some examples of how therapists can better justify treatments
- Detailed Documentation: Keep thorough notes on initial assessments, patient goals, progress, and adjustments made during therapy. Document each session’s activities and outcomes to show the treatment plan’s necessity and effectiveness.
- Evidence-Based Practice: Use research-backed techniques and explain how each method addresses the patient’s specific condition or symptoms. This strengthens the validity of chosen interventions.
- Functional Goals: Link therapy goals to the patient’s daily activities or specific functional improvements. For example, if a patient struggles with balance, the treatment should highlight how it improves their ability to walk independently.
- Outcome Measures: Regularly use standardized tests (e.g., range of motion, pain scales, functional scores) to track and document improvements, making it clear how the patient is progressing.
- Patient Education: Explain to the patient why each treatment is essential. When patients understand the purpose, they’re more likely to engage, which can be reflected in documentation as patient adherence.
- Consistency in Reassessment: Routinely reassess and update the treatment plan based on patient progress, showing a clear need for ongoing therapy or adjustments.
- Insurance-Ready Language: When justifying for insurance purposes, ensure documentation matches the language insurers use to support medical necessity, showing measurable outcomes and improvements.
Examples of Physical Therapy Documentation
Providing examples of physical therapy documentation examples can illustrate how best practices and proper documentation techniques are applied in real-world scenarios. These examples include initial evaluations, daily notes, and progress reports, each serving a specific purpose in capturing patient information and tracking progress.
Initial Evaluation Example
An initial evaluation provides a baseline status of the patient at the start of therapy and outlines the plan of care. For instance, Henry Smith, born on 3/22/1957, with a medical diagnosis of M17.12 Left knee OA s/p TKA, presents with decreased range of motion and strength, poor balance, increased swelling, and pain during functional activities. The treatment goals include returning to work as a supervisor and walking without a walker or cane, with treatments involving therapeutic exercise, neuromuscular rehabilitation, manual therapy, cold pack, and a home exercise program.
Such detailed documentation ensures that all aspects of the patient’s condition and treatment plan are clearly recorded, providing a solid foundation for future sessions and assessments.
Daily Note Example
Daily notes capture details of each therapy session, tracking treatments performed and patient responses. For example, in a daily note for Henry Smith, objective findings include ambulating with modified independence using a cane, vital signs, and a negative Rhomberg test. Subjectively, Henry reports a pain level of 3/10 and improved mobility after attending 13 treatments.
The treatment plan includes continuing the current exercise regimen, increasing the intensity of core strengthening exercises, and introducing functional activities. This level of detail ensures that each session is well-documented, providing a clear picture of the patient’s progress and any adjustments needed in the treatment plan.
Progress Note Example
Progress notes summarize the patient’s improvement and modifications needed in the treatment plan. For instance, Henry Smith has shown improvements in endurance and overall strength but lacks full strength to ascend a full flight of stairs. Treatments received include therapeutic exercise, neuromuscular re-education, manual therapy, cold pack application, and a home exercise program.
Future plans include addressing long-term goals with strategies such as strengthening exercises to increase quad activation, with progress assessments based on established physical therapy treatment goals.
This comprehensive documentation helps track patient progress over time, ensuring that treatment plans are adjusted as needed to achieve the best outcomes.
Enhancing Compliance and Legal Protection
Proper documentation is essential for enhancing compliance and legal protection. Detailed, organized records outlining treatment rationales, patient progress, and interactions are important for audit-proofing physical therapy documentation. This ensures that therapists adhere to treatment protocols and professional standards, providing a defense against legal liabilities and demonstrating that appropriate care was provided.
HIPAA Compliance
Adhering to HIPAA regulations is crucial for maintaining patient confidentiality and security. Physical therapists must keep all patient information confidential and secure to comply with HIPAA and foster trust.
Following APTA guidelines aids therapists in producing accurate and compliant documentation, reflecting clinical reasoning and ensuring quality patient treatment. By adhering to these standards, therapists can maintain high-quality documentation that meets legal and professional requirements.
APTA Documentation Standards
The American Physical Therapy Association (APTA) provides guidelines for physical therapy documentation to ensure it reflects clinical reasoning, patient interaction, and the course of treatment. These standards emphasize the need for accuracy and thoroughness in patient records, ensuring that all aspects of care are documented clearly and comprehensively.
By following APTA documentation standards, therapists can ensure that their documentation is defensible and meets professional and legal requirements. This not only enhances patient care but also protects therapists from potential legal issues.

Addressing Special Cases in Documentation
Special cases in physical therapy documentation require tailored approaches to ensure accurate records and compliance. Complex cases necessitate more detailed documentation to capture all relevant aspects of the patient’s condition and treatment.
Adapting documentation practices to specific patient scenarios ensures comprehensive care and meets legal requirements.
Pediatrics
When treating minors, it is crucial to follow specific documentation requirements that differ from those used for adult patients. Documentation for pediatric patients should include developmental milestones and any unique physical therapy considerations for that age group. Parental consent and participation must be documented in the treatment plan, ensuring that guardians are involved in the healthcare decision-making process.
These additional details ensure that the care provided is appropriate for the child’s developmental stage and that parents are fully informed and involved in the treatment process.
Cognitive Impairments
Thorough documentation is crucial in cases involving cognitive impairments as it helps tailor treatment approaches and supports patient care. Documenting for patients with cognitive impairments requires extra diligence due to variability in patient capacities and communication challenges.
Essential documentation elements for cognitive impairments include specific cognitive assessments, patient responses, and any observed behavioral changes. Utilizing structured templates and consistent terminology can enhance clarity and effectiveness in documentation for cognitive impairments.
Home-Based Therapy
When documenting home health therapy, it is important to include details about the home setting and any adjustments made to accommodate safety and communication. Documentation for home-based therapy should include details about the home environment and any safety concerns noted.
Effective documentation should also highlight communication with caregivers about the therapy process and any changes in the patient’s status. This ensures that the therapy provided is safe and effective, taking into account the unique challenges of the home setting.
Summary
Efficient physical therapy charting is essential for ensuring quality patient care, legal compliance, and operational efficiency. By understanding the key components of documentation, leveraging technology, and adopting best practices, physical therapists can enhance the accuracy and effectiveness of their charting. Implementing these strategies will not only improve patient outcomes but also protect therapists from potential legal issues. Remember, thorough and accurate documentation is the cornerstone of successful physical therapy practice.
Frequently Asked Questions
Why is physical therapy documentation important?
Physical therapy documentation is essential for legal compliance and accurate billing, as well as for maintaining continuity of care among healthcare providers. This ensures that patients receive consistent and effective treatment.
What are the key components of physical therapy documentation?
The key components of physical therapy documentation are patient details, medical diagnosis, treatment goals, and the plan of care. Ensuring these elements are well-documented is crucial for effective patient management and continuity of care.
How can technology improve physical therapy documentation?
Technology significantly improves physical therapy documentation by enhancing efficiency and reducing errors through tools like EMR software and voice-to-text systems. This streamlining allows for more accurate and accessible patient records.
What is the SOAP note format, and why is it used?
The SOAP note format, consisting of Subjective, Objective, Assessment, and Plan, is used for organized and comprehensive documentation of patient care, ensuring clear communication among healthcare providers.
How can physical therapists avoid common charting mistakes?
To avoid common charting mistakes, physical therapists should ensure they include comprehensive subjective information, refrain from making assumptions, and develop detailed action plans. This approach will enhance the accuracy and effectiveness of their documentation.